What is a Retinal Tear?
 A retinal tear is a tear in the fabric of nerve tissue, called the retina, that lines the inside of the eye. Retinal tears typically occur at the thin edge of the retina. Tears are seen in two forms — a triangular horseshoe tear and a circular tear that often has a small divot of retina floating over the circle (operculated hole).
A retinal tear is a tear in the fabric of nerve tissue, called the retina, that lines the inside of the eye. Retinal tears typically occur at the thin edge of the retina. Tears are seen in two forms — a triangular horseshoe tear and a circular tear that often has a small divot of retina floating over the circle (operculated hole).
The vitreous jelly inside the eye sticks more firmly at the edge of the retina and "tugs" while it is being peeled off. This tugging is the cause of flashes, and if the tugging is strong enough, a retinal tear may develop. If a retinal tear occurs in the location of a retinal blood vessel, the blood from such a torn vessel leads to a showering of new floaters (vitreous hemorrhage).
What is a Horseshoe Tear?
A horseshoe tear is a retinal tear characterized by a flap-shaped tear resembling a horseshoe. It occurs when the vitreous gel inside the eye pulls away from the retina. This pulling creates a flap in the retina, leading to vision changes if untreated. Horseshoe tears can potentially evolve into retinal detachments, necessitating prompt diagnosis and management.
The Causes of a Horseshoe Tear
Horseshoe tears are primarily caused by the vitreous gel inside the eye shrinking and pulling away from the retina as part of the natural aging process. This traction can sometimes cause the retina to tear in a horseshoe shape. Factors that increase the risk include age, nearsightedness, and previous eye surgeries or traumas.
Treating Horseshoe Retinal Tears
Treating a horseshoe retinal tear typically involves procedures to seal the tear and prevent retinal detachment. The most common treatments include laser photocoagulation and cryopexy. These treatments help prevent fluid from accumulating under the retina, which can lead to detachment.
How Are Retinal Tears Treated?
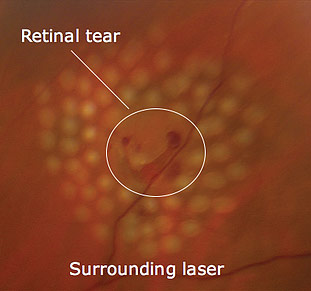 All new or old tears associated with sudden flashes and/or floaters require prompt treatment. The object of treatment for a retinal tear is to create a firm adhesion, called a retinopexy, between the retina and the wall of the eye so that the liquefied vitreous cannot pass through the tear and then dissect underneath the retina and cause a retinal detachment. Such an adhesion is usually formed by creating a circle of small scars around the tear with a laser.
All new or old tears associated with sudden flashes and/or floaters require prompt treatment. The object of treatment for a retinal tear is to create a firm adhesion, called a retinopexy, between the retina and the wall of the eye so that the liquefied vitreous cannot pass through the tear and then dissect underneath the retina and cause a retinal detachment. Such an adhesion is usually formed by creating a circle of small scars around the tear with a laser.
Sometimes, if the view of the retina is poor, e.g., from a dense cataract or blood in the vitreous cavity, the adhesion is created using a metal probe cooled to -20°C. This freezing metal probe, called a cryoprobe, is placed against the eye wall underneath the tear, where the local inflammation caused by the freezing creates the desired adhesion. A similar process using a transcleral diode laser can also achieve the same result.
For the Spanish version, click here ›
For the Spanish version, click here ›
Retinal Tear vs. Retinal Detachment
A retinal tear is a break in the retina that allows fluid to enter under the retina. If untreated, a tear can lead to a retinal detachment, where the retina separates from the back of the eye, potentially leading to severe vision loss or blindness. Retinal detachment is more severe and requires immediate medical attention, whereas retinal tears might be treatable with less urgent procedures to prevent detachment.
What Is a Retinal Detachment?
A retinal detachment is a separation of the retina's nerve tissue from the eye's wall. When this separation occurs, the cells of the nerve tissue are isolated from their supplies of nourishment, will deteriorate, and eventually die. Therefore, a retinal detachment must be repaired to prevent permanent loss of vision in the affected eye.
Rhegmatogenous Retinal Detachment
The most common type of retinal detachment is called a rhegmatogenous retinal detachment. Rhegmatogenous retinal detachments occur when fluid from the vitreous cavity flows through a retinal tear and dissects underneath the retina, thus raising it off the wall of the eye. Similar to the posterior vitreous, the retina is only firmly attached to the wall of the eye at the optic nerve and at the far peripheral edge of the retina. The rest of the retina is attached to the wall of the eye in a fashion similar to a suction cup. Once a small amount of fluid gets underneath the retina, the "seal" is broken, and the dissecting fluid can spread rapidly.
Symptoms of Retinal Detachment
The initial symptoms of a retinal detachment are the same as a retinal tear or a posterior vitreous detachment, i.e., flashes and floaters; however, as the detachment progresses, a dark, opaque, moon-shaped shadow or curtain will appear from one side of your vision. This curtain, which can sometimes be seen to billow like a sail in the wind, is actually the detached retina tissue floating in the vitreous cavity.
The Severity of Retinal Detachment
Retinal detachments can be divided into two levels of severity—macula on and macula off—depending on whether the detachment affects the very important back portion of the retina, called the macula.
Since retinal detachments tend to start in the periphery as "macula on" retinal detachments and only later progress to "macula off" retinal detachments, the prognosis for the return of normal vision after the repair of a "macula on" detachment is better. In addition, "macula off" detachments that are less than a week old tend to have a better visual prognosis than older "macula off" retinal detachments. Since retinal detachments tend to start in the periphery as "macula on" retinal detachments and only later progress to "macula off" retinal detachments, it is very important to seek out an ophthalmologist immediately upon the earliest detection of the suspicious symptoms outlined above.
Fortunately, over 90% of all retinal detachments can be repaired with modern surgical techniques. Current methods can be performed as outpatient surgeries or even in the office.
Other Types of Retinal Detachment
Besides rhegmatogenous retinal detachment, the other retinal detachments — tractional and serous — behave very differently. Tractional retinal detachments typically occur when scar tissue within the eye pulls the retina away, often seen in advanced diabetic retinopathy cases. On the other hand, serous retinal detachments involve fluid accumulation under the retina, resembling a blister. This type of detachment can arise from various conditions, including inflammatory diseases, tumors, or other eye diseases.
How Are Retinal Detachments Repaired?
Most retinal detachments require urgent surgical repair. The object of retinal detachment repair is to get rid of the fluid underneath the retina and allow the retina to lay “flat” upon the concave contour of the eye wall. There are several methods of achieving this goal, each of which will be discussed in the sections below. Most retinal detachments are of the rhegmatogenous type, and these sections will primarily discuss the repair of this type of detachment.
There are three ways to repair a rhegmatogenous retinal detachment:
- Scleral buckle
- Pars plana vitrectomy
- Pneumatic retinopexy
